
Despite what many believe, the most critical window for knee rehabilitation after surgery such as ACL, meniscus, or joint replacement, isn't months later, it's in the first few days. This is a time when most patients are doing too little, not too much.
I see this happen all the time in my kinesiology studio. Clients come to me weeks or months after their knee surgery, frustrated because they're still weak and struggling with basic movements. When I ask about their early recovery, the story's always the same: "I heard I should rest and take it easy for six weeks."
Here are the key takeaways:
Early Movement Beats Extended Rest: The most critical window for knee strengthening is the first few weeks after surgery, not months later. Your body starts losing muscle mass within days, so move as soon as your surgeon allows rather than waiting weeks.
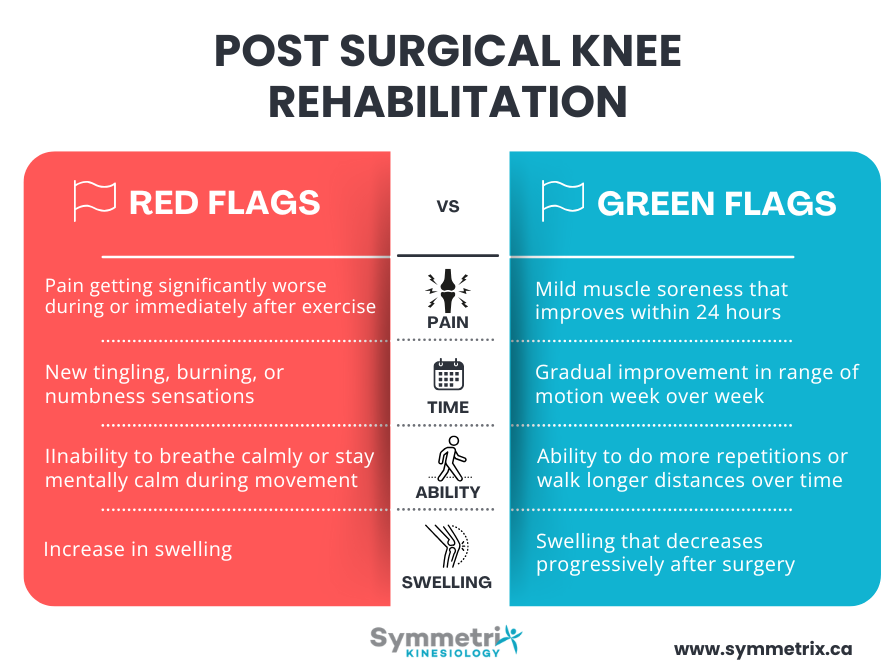
Know Your Pain Signals: Learn the difference between safe discomfort and warning signs. "Know pain, know gain" means understand what sensations are normal versus red flags like significantly worsening pain, tingling, or inability to breathe calmly during exercise.
Individual Assessment Trumps Generic Programs: There are some great ACL and other knee injury cookie-cutter programs out there, but identifying your specific weaknesses and movement patterns is more effective than following preset protocols. Professional assessment can shortcut your recovery by seeing compensation patterns you can't detect yourself.
Pacing Prevents Setbacks: Establish a baseline level of function you can safely do on any day, then slowly build up. This prevents the crash-and-burn cycle that actually decreases function over time and keeps you stuck in the pain-fear loop.
The truth about post-surgical knee recovery challenges everything most people believe about healing. We've been taught that rest equals recovery, but science shows us something completely different. Your body needs movement and gentle loading to heal properly, not weeks of inactivity.
By the way, Symmetrix is currently accepting clients to our knee rehabilitation program. Book a free consultation with a kinesiologist to learn more.

What Rehabilitation Exercises Are Safe After Knee Surgery?
The key thing to remember is that each surgery is gonna be a little bit different. Listen to your surgeon in terms of limitations or restrictions. My rule of thumb is if you can weight bear, you can start doing basic movements like walking and modified squats.
Immediate Phase (First 24-48 Hours):
- Walking as tolerated: if you can weight bear, you can start walking
- Basic range of motion: gentle knee bending and straightening
Early Phase (Days 3-14):
- Wall squats or supported squats with limited range
- Light resistance band exercises for knee flexion and extension
- Straight leg raises to activate muscles without joint stress
Progressive Phase (Weeks 2-6):
- Bodyweight squats with increasing depth
- Step-ups starting with low steps
- Water-based exercises if available
- Eccentric exercises that work muscles while they're lengthening
The Truth About Post-Surgical Knee Exercise Timing
Why "Wait 6 Weeks" Advice Often Backfires
That six weeks you're waiting? You're actually losing muscle mass and function. Your body needs physical load for it to know which way to lay down the proteins in your tendons, muscles, and tissues.
I like this analogy: when we first cut our skin, we get just a random scab. That scab has proteins and sticky stuff that's aligned in all random directions. Then over time, as that scab heals, it gets replaced by new skin. That new skin, because of the stretching and movement of the body, is aligned in the right direction and isn't just like a big lumpy scar.
Internally, it's the same thing. You need that strain and stress for your body to understand how to heal properly. Without movement, your tissues heal randomly instead of in the strong, organized pattern you need for function.
The Critical First Hours for Movement
Surgeons now usually recommend that people move right away after most surgeries. Movement right away within a reasonable range of tolerance when done safely.
As a kinesiologist I'm seeing people not right after surgery because they've got physio at the hospital. The physio is usually leading clients through early activation, and then we as kinesiologists see people a few weeks post surgery. But we're almost always recommending to them to get moving as soon as they can.
You can actually start gentle movements almost immediately after most knee surgeries, even while you still have some pain. The key word here is "gentle." Your body is smart and it will tell you if you're doing too much too soon by making pain signals louder.
Surgical Type-Specific Timeline Differences
There is no exact timelines for different knee surgeries so I defer to the surgeon. Each surgery is gonna be a little bit different and it also depends if someone is having post-surgical complications like infection, they have another condition, etc…
If your surgeon is telling you not to do movement or kinesiology, then there's probably a really good reason for that. But in the best case scenario, the general rule is: move as soon as you can, within your tolerance.

Knee Rehabilitation After Surgery: What Actually Works
Early Activation vs. Extended Rest
Early activation is the best early-stage treatment. I expect that the physio in the hospitals are doing the same thing we recommend which is getting people moving as soon as possible.
During the first two weeks, your focus should be on pain management, restoring basic range of motion, and reactivating those stabilizing muscles around your knee. You will generally begin with gentle movements like quad sets, straight leg raises, and heel slides.
Post-Surgical Rehabilitation That Builds Real Function
When I’m working with knee surgery clients my strategy is identifying that specific person's weaknesses and then working on those weaknesses. Generally speaking, we work on squats, deadlifts, lunges. The muscles involved with these are quads, hamstrings, calves, and bridges for glutes.
But the specificity matters, does their coordination need work? Do their hip flexors need work? Is there one side that needs more work than the other? A lot of the time it does because knee surgery is usually done one side at a time.
I prefer doing mobility work through what we call "eccentric strengthening" which means getting your muscles to work while they're lengthening. This gives you range of motion improvements while also building strength, rather than just static stretching.
Progressive Loading Principles for Surgical Recovery
Each person is gonna be really different. Some people can handle a lot more load than other people, and I would just say listen to your body. Your body will very much tell you how much it allows you to do.
Let me share a real example. My most recent knee replacement patient actually just had surgery six days ago. He called me a few months ago, and his acupuncturist recommended he come see us before surgery. We started with aquatic therapy. We did a lot of water running to get him to work his legs without putting pressure on the joint.
We also did a gym program that focused mostly on upper body and core so he could maintain strength without loading the legs too much, because that tended to make his knee worse. I found it interesting that in the three months we worked together, his knee function actually improved in the gym as well. He was able to start doing wall squats and had a functional range of about 90 degrees as his legs got stronger.
The joint actually felt better for him, and I think that's because he gained more strength in his legs and the joint was more supported. Now he's had his knee replacement, and once he's done with his hospital physio, he'll be back.
We'll start working primarily in the gym now that he’s had his surgery. I’ll help him to strengthen his legs and work on function. He's got a global trekking adventure that he's working towards in November, so we've got about four months to prepare for that.
Post-Op Knee Rehabilitation Myths That Keep You Weak
"No Pain, No Gain" vs. "Complete Rest" - Both Are Wrong
I believe in "know pain, know gain" rather than "no pain, no gain". K-N-O-W your pain, know gain. We need to understand what kind of sensations we're getting and whether it's a safe pain to move through or whether it's not a safe pain to move through. I wrote a blog post about know pain know gain, it’s a big topic.
No pain, no gain is the traditional saying but tends to push people towards a crash and burn. They do too much and then they end up getting a big pain flare-up, and then they have to slow rehabilitation. That approach over time decreases function because we end up doing too much, crashing and burning, and next time not being able to do quite as much because our nervous system becomes more sensitive.
The opposite approach is waiting until the pain goes away, waiting until things feel better to start doing anything. That also doesn't work because you end up losing muscle mass, losing function, and by the time you start rehab you are significantly weaker. If you wait you have a longer recovery time.
The Truth: The best approach is somewhere in the middle, balancing both worlds through pacing.
Pacing is establishing a level of function, a baseline level of function that you feel safe to do on a good day or a bad day, on any day basically. Then slowly building that up gently over time. That might look like "I am able to do 10 squats today," so maybe we do 10 squats tomorrow and over time build that up to 11, to 12.
Why Ice and Elevation Aren't Enough for Recovery
There was the old acronym RICE: Rest, Ice, Compression, and Elevation. That's actually old news now. I do think ice can be helpful. Ice and compression and elevation help with swelling in the first few days.
But these days, the acronym is POLICE: Protection, Optimal Loading, Ice, Compression, and Elevation.
Protection means while we wait for the stitches to heal, we may not want to push the joint into range of motion that might tear the stitches out. In general, just going slow with range of motion and only going as far as the body will let you go.
Optimal Loading - that O and L - speaks to starting to move, starting to put weight into the joint. The ice, compression, and elevation are still there, but prioritized appropriate loading which is crucial.
Surgical Knee Recovery: What Doesn't Work (And Why)
Cookie-Cutter PT Programs That Ignore Individual Needs
There's definitely lots of cookie-cutter programs out there and some of them are really good. For example there is a great resources for ACL recovery called The Melbourne ACL Rehabilitation Guide 2.0 that gives you week-by-week types of exercises to do and what kind of things you need to be able to do to move to the next level. For example, being able to do 20 single-leg squats before you're going into jumping.
One thing with these programs is it's tricky to assess ourselves. It's hard to know exactly what is happening within our own bodies.
I definitely think starting to move and get exercising is great if you can't afford care or don't have care available where you live. But if you're living in a major city and you've got physios and kinesiologists and other people around you to help you, and if it’s within your budget, I definitely think professional care is a shortcut.
Each knee surgery is going to be so different, and each person compensates in their own unique ways. You end up having an assessment and you learn things that you can't see on your own. Your kinesiologist may prescribe more specific exercises to you and your specific condition that you wouldn't know about or that aren't cookie-cutter.
When someone comes into our clinic, I take them through a comprehensive assessment process. I'm looking at how you squat, how you deadlift, are there any barriers to these activities, what is your functional ability right now? Based on what I observe, I'm marking things down and looking for imbalances.
Passive Range of Motion Without Active Movement
Passive range of motion can work, it really depends on what someone is working on and if maybe they're so limited that their muscles aren't working that well yet. Passive range of motion will create stretch on the tissues, which will be some load.
In terms of rehabilitation, you need to activate your muscles. That muscle activation will create the load that you need to get stronger and more functional.
I find that a lot of people make the mistake of only stretching, especially at the beginning of their rehab. I believe we can manage pain through gentle movement and building strength rather than just static stretching.
Avoiding Weight-Bearing Too Long
Weight-bearing can be a really good starting spot. Your bones, muscles, and joints need load to stay strong and healthy. When you avoid putting weight through your leg for too long, everything starts to weaken.
Red Flags vs. Normal Discomfort in Post-Surgical Rehabilitation
When Pain Signals Problems
If you're doing something and your pain is getting significantly worse as you're doing it, I would stop and pause and reassess. If your pain is getting significantly worse, your body is trying to tell you something.
If you can't breathe calmly or stay calm in your mind through doing something, then I would also question whether you should be doing that. You should be able to breathe and generally not hold a lot of tension in your body as you're doing exercise.
If you're getting more sensations of tingling, burning, numbness, or there's a lot more pain and swelling, I would also say those are red flags.
Learning the difference between pain signals you should pay attention to and normal exercise discomfort is probably one of the most important skills in recovery.
Expected vs. Concerning Swelling Patterns
Definitely after surgery, there's gonna be some expected swelling. But it should progressively get better as you're moving away from the surgery date. As more time passes, it should improve.
Normal Swelling Pattern:
- Peaks in first 2-3 days post-surgery
- Gradually decreases over 2-4 weeks
- May increase slightly after activity but returns to baseline
Concerning Swelling Pattern:
- Suddenly increases weeks after surgery
- Doesn't respond to rest, elevation, or ice
- Accompanied by redness, warmth, or fever
Signs Your Rehabilitation Program Is Working
Your function should get better. Over time, you should be able to do more. More repetitions, more range of motion, or more sets of things. You should be able to bend your knee deeper, be able to walk longer and longer distances, and just feel more comfortable with movement in general.
The improvements might be small day to day, but when you look back over weeks, you should see clear progress. If you're not seeing any improvement after 2-3 weeks of consistent effort, or if you're getting worse, that's when you need to reassess your approach.
Whether you're recovering from ACL surgery, meniscus repair, or knee replacement, the principles remain the same: move early, progress gradually, and focus on rebuilding function rather than just managing pain. Your knee surgery doesn't have to define your long-term strength and mobility, but the choices you make in those first critical weeks absolutely will.
Symmetrix is currently accepting clients to our knee rehabilitation program. Book a free consultation with a kinesiologist to learn more.

.jpg)






